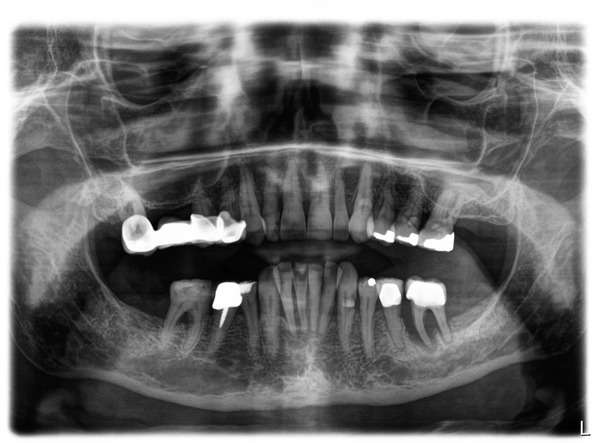
A female patient in her 70s attended the practice in 2019 in substantial dental pain. She also had a loose LL6 tooth and was missing her LL7 and LL8. An initial assessment was conducted, revealing a hopeless prognosis for the LL6, which was extracted as part of the emergency appointment. The patient was keen to continue her dental journey by restoring the gaps in her dentition, so we scheduled for her to return three months later for a comprehensive evaluation of the restorative options available.
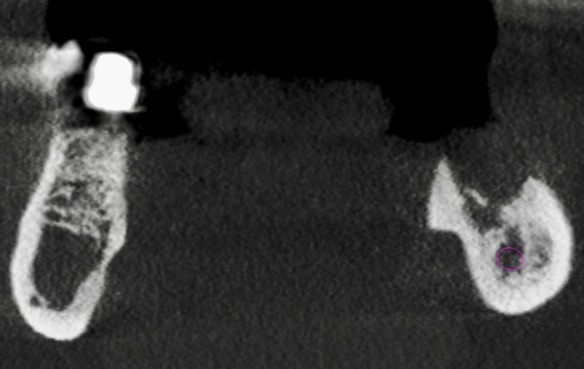
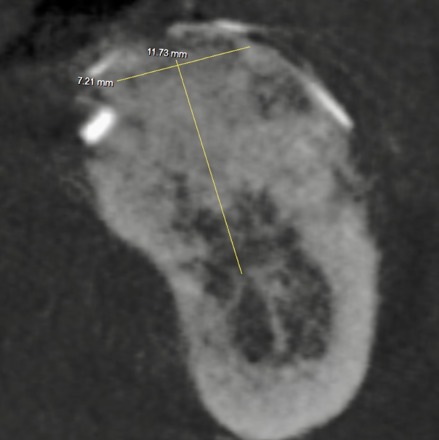
A CT scan demonstrated significant horizontal and vertical bone loss in the area, putting the alveolar crest very close to the dental foramen and alveolar nerve. This did not mean that dental implants were not possible, but additional considerations would be required. For example, with only 3mm of bone, short implants were not an option. This left us a choice between implant placement with nerve lateralisation in order to create sufficient space for restoration, or implant placement alongside vertical bone augmentation with a block graft or particulate bone and a PTFE membrane.
All these treatment options were discussed in full with the patient, as were no treatment and dentures as other possibilities. She expressed a preference for an implant with bone augmentation so that she may enjoy the benefits of a long-term fixed restorative solution.
A full suite of clinical photographs, radiographs and a CT were taken to inform the treatment plan. These were used to digitally plan where bone grafting would be most important, as well as the final position, angle and depth of implant needed to facilitate stable, functional and aesthetic restorations. The plan also incorporated a soft tissue graft, which would be performed after bone augmentation and implant placement following a staged approach for the best result in this case.
The advantages, limitations and risks of each procedure involved were outlined and the importance of oral hygiene emphasised before the patient gave fully informed consent to proceed.
A staged treatment approach
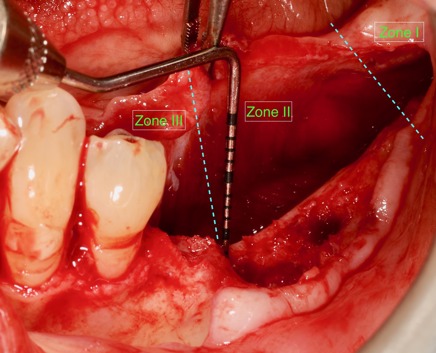
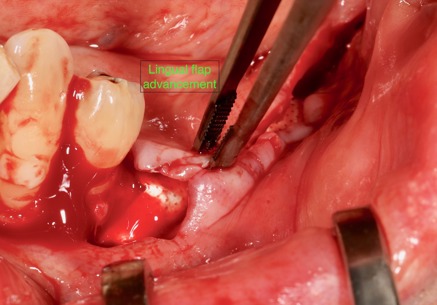
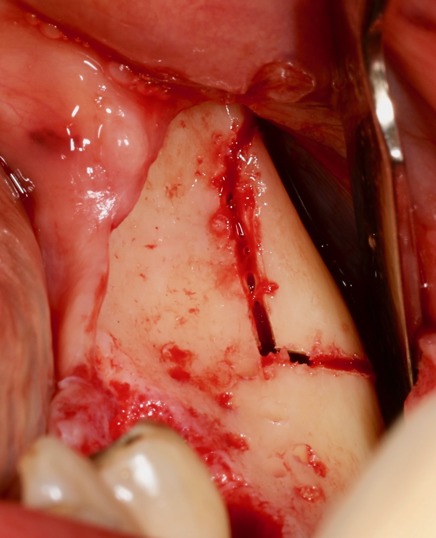
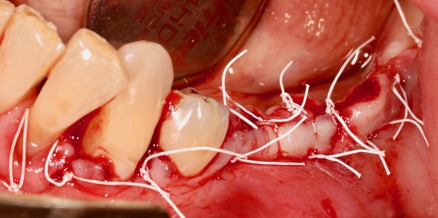
On the day of surgery, a safety flap was raised and extended two teeth away from the defect mesially. One crestal incision was made in the keratinised mucosa and one oblique incision made towards the coronoid process. I used a modified lingual flap technique that is divided into three different zones and steps; the first is the retro molar region, the second the high mylohyoid muscle attachment area, and the third is low mylohyoid muscle attachment area. By working in three separate regions, this allowed the use of three different techniques to advance the lingual flap without damaging the vital structures behind, including the lingual nerve and submandibular glands.
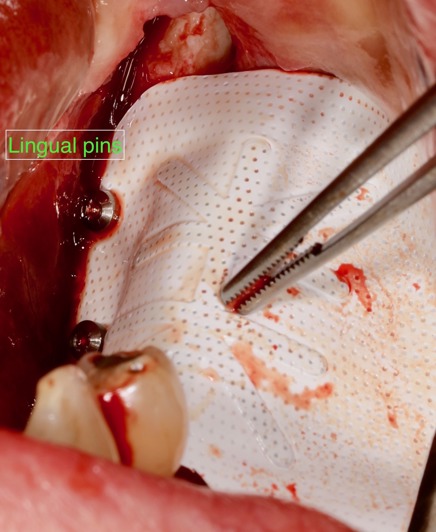
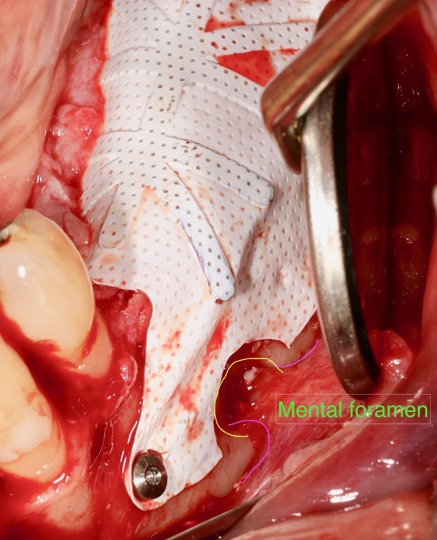
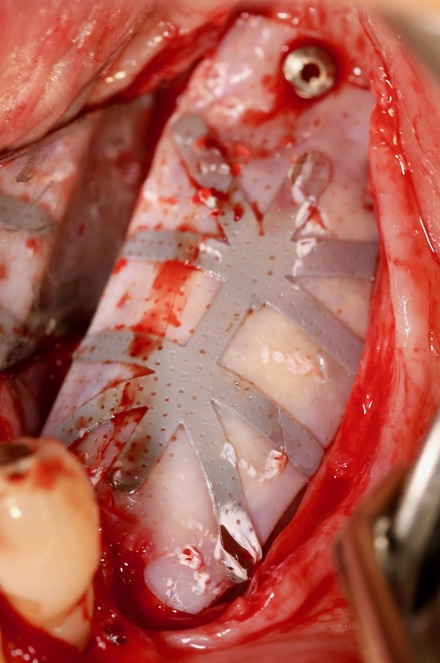
Once the buccal and lingual flaps were raised, autogenous bone was harvested from the ramus of the mandible using a piezomed instrument and a safe scraper. The harvested bone was particulated using a bone mill. The bone graft was prepared with 60 per cent autogenous bone and 40 per cent xenograft. A PTFE membrane was selected, shaped and secured into place with master pins inserted lingually first. The graft was loaded into the defect, with the membrane folded buccally and secured with further master pins.
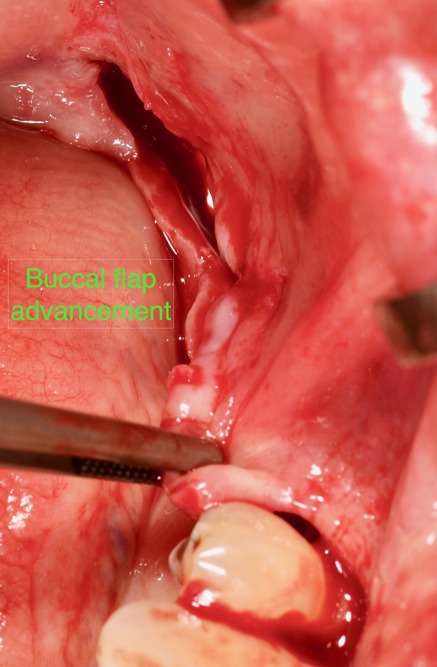
The buccal and lingual flaps were checked for passive closure, and it was decided to further release the buccal flap by using a mucoperio elastic technique. The soft tissue was then closed with PTFE sutures, ensuring the connective tissue met connective tissue. The patient was given standard post-operative oral hygiene and dietary instructions upon conclusion of the appointment.
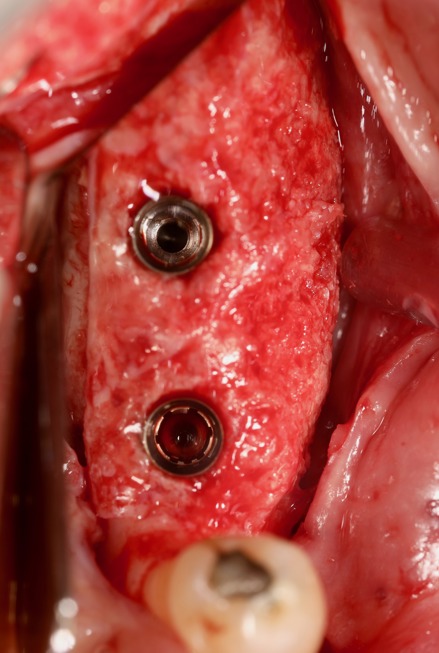
Approximately eight months later, the PTFE membrane was removed and two implants (4.2mm x 9mm) were placed in the pre-planned positions, angles and depths.
A further two months after this, the patient returned for a soft tissue graft designed to increase the amount of keratinised tissue around the implants. The strip graft technique was performed, using a free gingival graft tissue that was harvested from the palate. At the recipient site, a split thickness flap was raised and apically repositioned. The graft material was placed on top of the periosteum and left to mature for three months.
At this point, treatment was concluded with the restoration phase. The implants were exposed, impression copings placed and a new impression taken for the fabrication of the implant-retained crowns. These were fabricated and loaded.






Discussion
Treatment options were restricted in this case due to the lack of bone available. The size of the defect ruled out short implants immediately. Doing nerve lateralisation is also a high-risk procedure, so is often not the first-choice for patients. In addition, the crown would be too long compared to the neighbouring crown, so cleaning and maintaining the implant in the long-term can be difficult for the patient following this approach. The methods used instead were selected because they provided more predictable results. The modified lingual flap techniques also allowed us to advance the lingual flap enough to cover the graft for tension-free closure. This is essential for the soft tissue health, as well as the function and aesthetics of the implant in the long-term. The five-year follow-up of this particular case demonstrates the stability of the results achieved.
For more information visit www.ashaclub.co.uk

