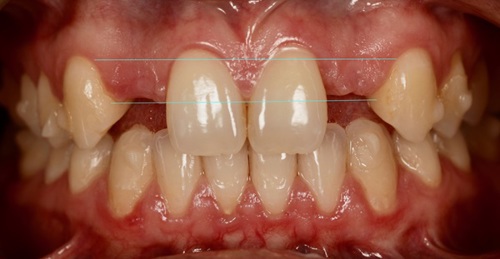
A female 30-year-old patient presented to the practice with congenitally missing lateral incisors. She was a non-smoker, her medical history confirmed her to be generally fit and well and her oral hygiene was in good condition. The patient had a fixed bridge in place, but reported that this was continually debonding every six months or so. Given that this type of restoration wasn’t working for her, she was seeking a more permanent solution in the form of a dental implant. The patient also informed us of her upcoming wedding, for which she hoped to have all dental treatment complete in time.
A comprehensive clinical assessment was conducted to determine suitability for implant treatment, including a full suite of clinical photographs and an intraoral impression. A medium-high lip line was noted, which would make the avoidance of black triangles important to the final outcome. It was also established that the existing spaces were very narrow, which indicated that orthodontic treatment would be required prior to implant placement. This was discussed with the patient, along with detailing the potential implant therapy options post realignment, and she was very keen to proceed. A referral was made for Invisalign treatment to widen the spaces at the lateral incisor sites and the patient returned to the practice a few months later for full implant planning.
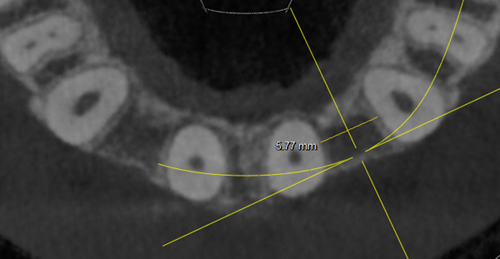
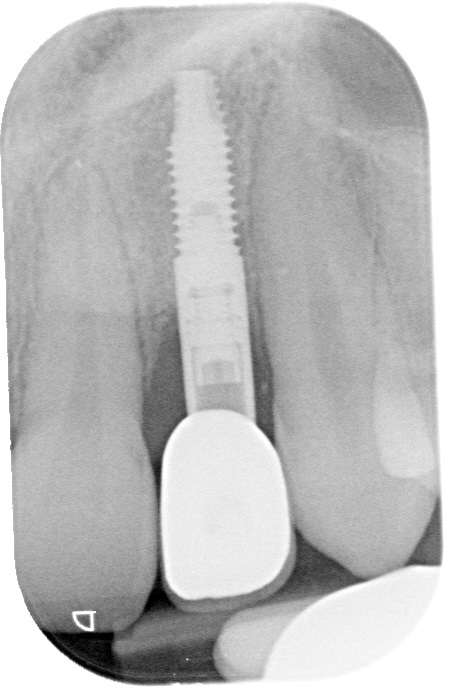
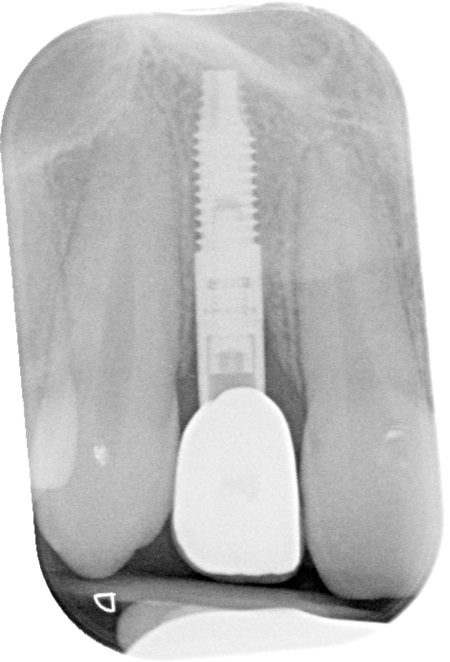
A radiograph and CBCT image were taken to show adequate width had been obtained for the placement of two lateral implants. However, there was a lack of bone buccally, indicating that bone augmentation would be necessary for successful implant treatment. Soft tissue grafting was also recommended in order to boost gingival volume and restore any height lost post-operatively for an ideal aesthetic (which was especially important given the medium-high lip line in mind).
A fully digital workflow was utilised to plan the ideal position, angle and depth of the implants, as well as the accompanying restorations. It was decided to use a guided surgical approach in order to increase the accuracy, predictability and efficiency of the procedure, encouraging a faster and more comfortable patient experience. This was particularly beneficial given the narrow area in which we were placing the implants.
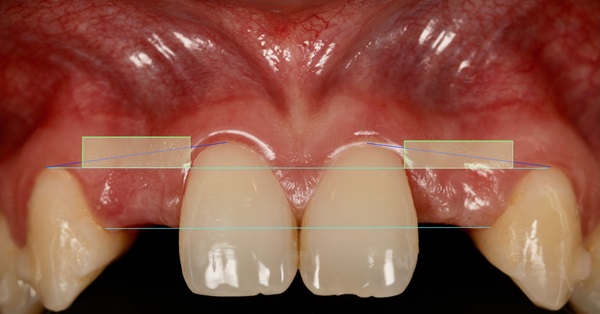
The diagnostic wax-up was created and shared with the patient as part of the consent process. Once the benefits, risks and limitations of treatment were discussed once again with the patient, informed consent was recorded to proceed.
The scans, diagnostic wax-up and photos were sent to the dental laboratory to fabricate the surgical guides.




Phase I: Surgical treatment with implant placement, soft and hard tissue augmentation
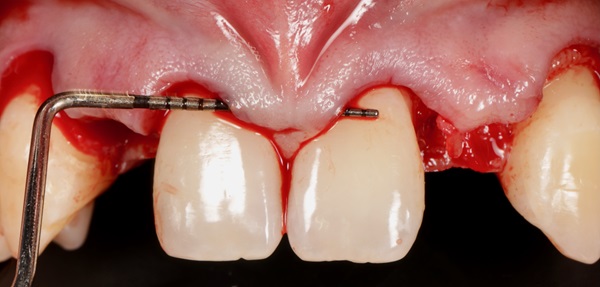
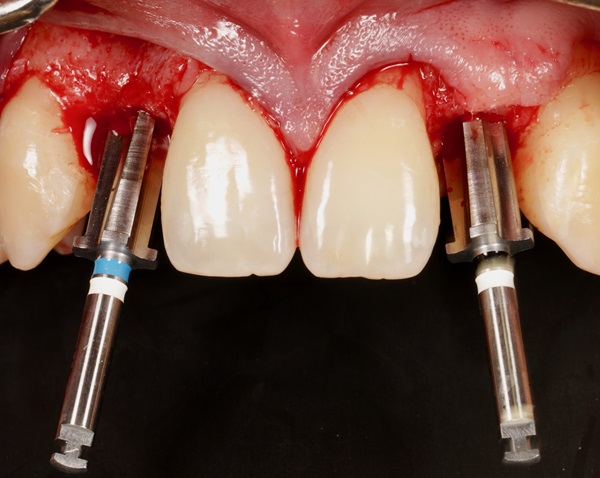
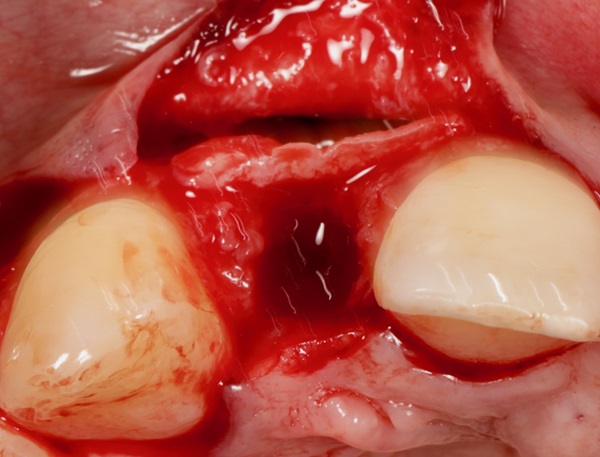
On the day of surgery, the patient was numbed with a local anaesthetic and a split-mucogingival, full thickness flap was raised. The surgical guide was fitted into the mouth and the two implants were placed through the guide to replicate the exact positions, angles and depths determined during the planning phase.
Bone was harvested from the left mandible and used to augment the implant sites. The bone grafting was performed by combining this autogenous bone with xenograft and using the ‘mini sausage’ technique. A collagen membrane was used to hold the graft material in place, secured with periosteal sutures.
Soft tissue was then harvested from the palate – enough for two connective tissue grafts (CTGs) at each lateral incisor location. The aim of these was to regain the soft tissue contour around the implant sites and build the papillae back up. This would not only reduce the soft tissue shrinkage that occurs post-surgery, but would actually increase the width of the papillae compared to where we started for optimal aesthetic results.
The flap was coronally advanced to increase root coverage and sutured closed. Upon conclusion of the surgery, the patient was given standard post-operative oral hygiene and dietary instructions, with particular focus on oral hygiene. She returned to the practice one week later for the post-surgical review, reporting no abnormal pain or discomfort. The sites also looked to be healing as expected.



Phase II: Restoration
The patient returned three months later for the restorative phase of treatment. The implants were exposed and the abutments and temporary crowns were fitted. These were designed to help contour the newly enhanced soft tissue and shape the papilla accordingly. They also provide an excellent trial for the patient, ensuring she was happy with the shape and colour of the crowns before the final restorations were fabricated in zirconia.
Both the patient and I were delighted with the outcome reached in this case. The patient achieved her primary aim of restoring the lateral incisors with a fixed solution that wouldn’t require adjustments or re-bonding every six months. We were also able to deliver a highly aesthetic and functional result with the use of soft and hard tissue augmentation.


Discussion
The planning for a case such as the above is crucial. It presents ‘double trouble’ in that the lateral incisor site is extremely difficult to place an implant into due to how narrow the space tends to be – and we were treating both lateral incisor sites. As such, this case was very aesthetically demanding, plus we had to consider the time restrictions imposed by the patient’s upcoming wedding. The soft tissue management was particularly important for the aesthetic outcome. This was made slightly simpler by the use of guided surgery, which ensured that the implants were placed accurately for the best results.
In conclusion, this type of case requires meticulous planning and sufficient skill with both bone and soft tissue grafting techniques. However, with adequate training it is possible for most dentists within the implantology fi eld to achieve an excellent result. I would recommend that colleagues have at least five years of experience with dental implants before moving onto situations that present the complexity that a double lateral incisor restoration offers.
For more information visit www.ashaclub.co.uk


