A 68-year-old female patient presented to the practice complaining about the appearance of her teeth. She had existing crowns in the UL1,2,3, in addition to a bridge in the upper right quadrant which was placed 10-15 years ago. The patient’s main concern was the marginal fit of the crown, and she felt that the bridge was too big.
A full medical history was taken, showing the patient to be generally fit and well. A clinical exam was conducted, requiring the bridge to be removed. This revealed hard and soft tissue defects in the UR2,3,4 region. The patient had a retained root on UR3, a failing crown on UR5 with marginal leakage and gingival recession, and was missing UR2,4,6 and LL6. An X-ray and CT scan were taken, in addition to creating study models. Digital treatment planning incorporated both the hard and soft tissue to enable us to achieve the optimal result. The CT scan confirmed a lack of bone and soft tissue, making this a challenging case to achieve a good result.
Treatment planning
The patient was presented with all of the appropriate options for treatment including replacement of the existing crowns to improve smile aesthetics, replacing the LL6 missing molar with a dental implant, and placing an implant retained bridge in the UR2,3,4 region. Due to the insufficient hard and soft tissue, a decision was made to place implants on UR3,4 with bone grafting and a connective tissue graft to enhance the gingival thickness and aesthetic outcomes in the upper right quadrant.
All aspects of the treatment were discussed with the patient in depth, including conversations about the benefits and risks. As the patient was particularly concerned about the aesthetic outcome, it was important to manage her expectations at this stage, to ensure she had a complete understanding of the limitations of the treatment. Once all the patient’s questions were answered and she was comfortable with treatment, she provided informed consent to proceed.








Treatment provision
The patient visited the restorative dentist Evangelos Viskadourakis (GDP at our practice) for the initial phase of treatment, in which the existing bridge and crown were removed. Following this, the patient was referred to me for implant placement at the LL6, and to restore the upper right quadrant with dental implants.
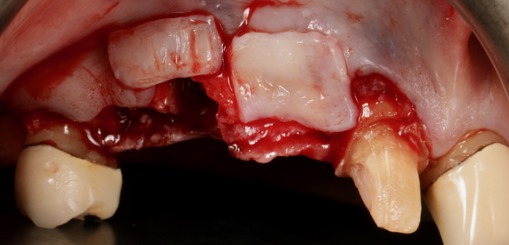
On the day of surgery, the upper right quadrant was numbed using local anaesthetic and a mucogingival split thickness flap was raised. The UR3 was extracted atraumatically and autogenous bone was harvested from the mandible to form a bone graft comprised of 60 per cent autogenous and 40 per cent xenograft material.
Two Sweden & Martina Prama dental implants were placed in the UR3 and UR4 locations at the predetermined position, angle, and depth. Bone augmentation was carried out in these areas following the ‘layering technique’ to ensure the graft attached effectively all around the implants for maximum stability.
Soft tissue was harvested from the patient’s palate and a connective tissue graft was then placed over the implant site to increase the gingival volume and build papilla. The flap was advanced to enable it to be closed tension-free. In the same appointment, the patient’s original the dental implants. The area was scanned and sent to the dental lab in order for them to create a provisional bridge.
On the same day, a dental implant was placed in the LL6, with a connective tissue graft was provided to improve soft tissue and papilla thickness, and a final crown was fitted.
After four months of healing, the bridge was removed and replaced with the lab-made provisional bridge. The aim of the provisional bridge was to encourage soft tissue contour. Three months later, the lab-made provisional bridge was removed and the final implant retained bridge and crowns were placed.
Following this, composite bonding was carried out in the lower anterior teeth in order to improve occlusion and enhance aesthetics.











Case reflection
The patient and clinician were both pleased with the functional and aesthetic outcome of this case. It demonstrates the need to listen to patients’ concerns attentively and ensure clear communication when it comes to expectation management, to ensure patients can provide fully informed consent and avoid disappointment. A key clinical challenge in this case was soft tissue contouring. This was not easy because the upper right quadrant required dental implants, whilst the upper left quadrant comprised of natural teeth and a crown. As such, it was difficult to match the two sides and achieve an aesthetic and still natural-looking outcome on both sides.
For more information visit www.ashaclub.co.uk


